Trauma / Fractures and Related Conditions

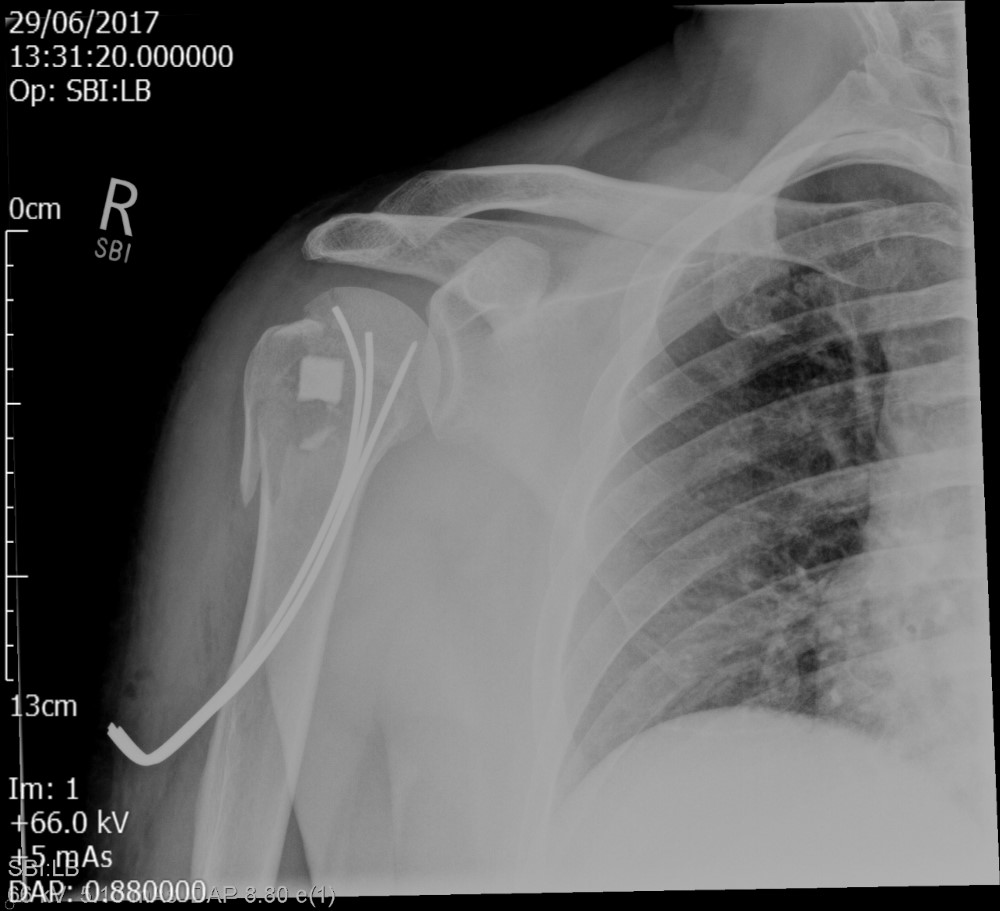
Proximal Humeral Fractures - Minimal Invasive Fixation
Minimally invasive fixation with modified palm tree technique for proximal humerus fractures: Outcomes in a series of 132 patients
Introduction: Various surgical techniques and implants are available for surgical treatment of significantly displaced proximal humerus fractures.We describe a minimally invasive technique using 3 curved wires, inserted in a retrograde fashion into the humeral head. These are aimed to diverge within the humeral head to provide three separate 3-point fixations to achieve good stability.We present the results of proximal humerus fractures managed with the modified palm tree technique.
Methods: A retrospective analysis of data collected prospectively including demographics, radiographs, clinical outcomes, complications and revision surgery for patients treated with the palm tree technique was performed.
Results: Between 1998 and 2017, 132 patients underwent fixation with this technique. Average age was 61.8 years. Fifty-Eight fractures were 2 part, 46 were three part and 28 were four part. Average follow up was 26 months. In three to four part fractures, a bone graft substitute block was used behind the humeral head fragment for structural support. There were 11 early revisions (8.3%). In 7 cases the fixation failed early and was revised to other implants like angular & locking plates (4), hemiarthroplasties (2) and reverse arthroplasty (1). In 4 cases the construct was revised to achieve better positioning of the wires. From the 125 remaining patients, 120 achieved union(96.8%). There were 3 painless fibrous non-unions and 2 painful non-unions requiring revision. The mean final Constant score was 75.5 and subjective shoulder value was 7.8/10. Nine patients (6.8%) developed avascular necrosis of the humeral head of which three patients were revised later to an arthroplasty.
Conclusion: This technique is a simple, minimally invasive technique which can be used for two, three and four part fractures with good functional outcomes and high union rates. No metalwork remains in the proximal humerus should another procedure like arthroplasty be required in case of avascular necrosis of the humeral head or fracture sequela.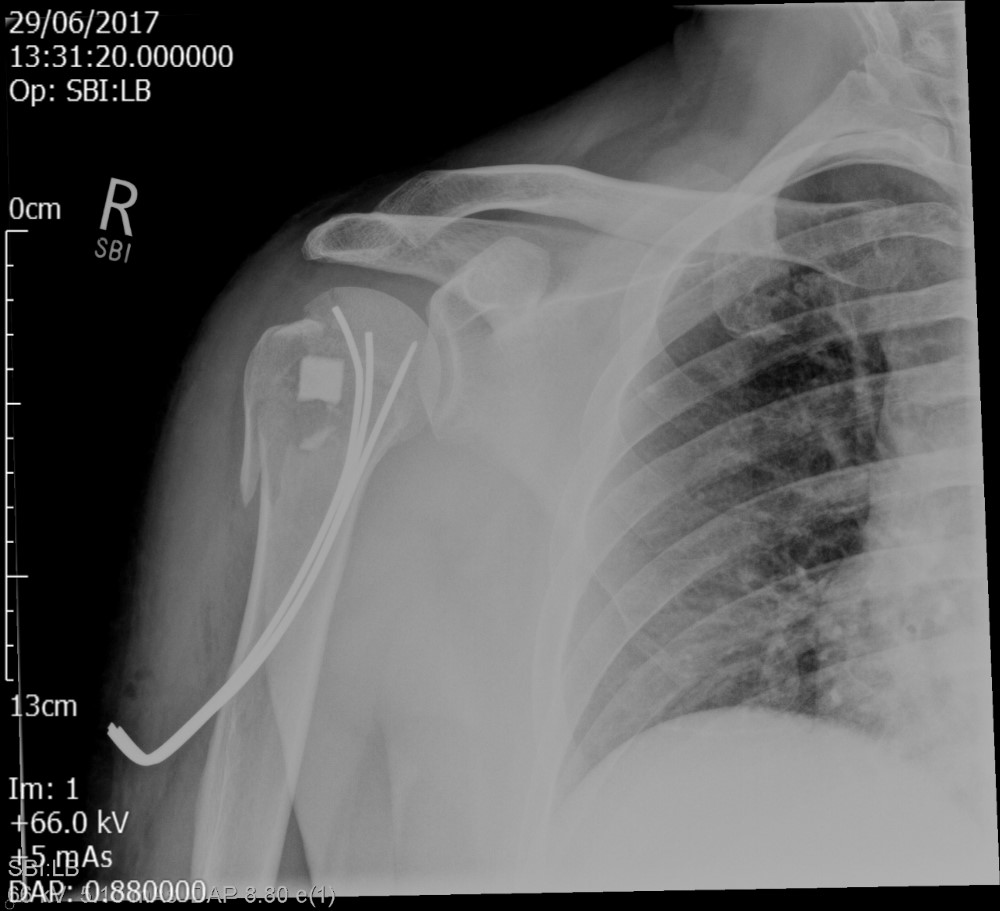
Introduction: Various surgical techniques and implants are available for surgical treatment of significantly displaced proximal humerus fractures.We describe a minimally invasive technique using 3 curved wires, inserted in a retrograde fashion into the humeral head. These are aimed to diverge within the humeral head to provide three separate 3-point fixations to achieve good stability.We present the results of proximal humerus fractures managed with the modified palm tree technique.
Methods: A retrospective analysis of data collected prospectively including demographics, radiographs, clinical outcomes, complications and revision surgery for patients treated with the palm tree technique was performed.
Results: Between 1998 and 2017, 132 patients underwent fixation with this technique. Average age was 61.8 years. Fifty-Eight fractures were 2 part, 46 were three part and 28 were four part. Average follow up was 26 months. In three to four part fractures, a bone graft substitute block was used behind the humeral head fragment for structural support. There were 11 early revisions (8.3%). In 7 cases the fixation failed early and was revised to other implants like angular & locking plates (4), hemiarthroplasties (2) and reverse arthroplasty (1). In 4 cases the construct was revised to achieve better positioning of the wires. From the 125 remaining patients, 120 achieved union(96.8%). There were 3 painless fibrous non-unions and 2 painful non-unions requiring revision. The mean final Constant score was 75.5 and subjective shoulder value was 7.8/10. Nine patients (6.8%) developed avascular necrosis of the humeral head of which three patients were revised later to an arthroplasty.
Conclusion: This technique is a simple, minimally invasive technique which can be used for two, three and four part fractures with good functional outcomes and high union rates. No metalwork remains in the proximal humerus should another procedure like arthroplasty be required in case of avascular necrosis of the humeral head or fracture sequela.
Scapular (Shoulder blade) Fractures